As healthcare continues to adopt value-based care (VBC) models, the role of pharmacists continues to evolve. Pharmacist-led initiatives can improve clinical outcomes, reduce costs, and meet all-important quality metrics for your program. But implementing pharmacist-led initiatives requires careful planning and flawless execution. Ideally, programs are built with pharmacists in expanded roles in mind, rather than retrofitted to accommodate them.
Let’s explore some best practices for implementing pharmacist-led initiatives in VBC programs.
Identify Where Pharmacists Can Have the Most Impact
Before implementing pharmacist-led initiatives in VBC programs, you must identify specific areas where pharmacists can make the most impact. Their expertise in medications and medication management is fundamental to their ability to impact health and financial outcomes. But these highly trained professionals also have the skill and experience to deliver high-quality, patient-centered care in other clinical areas. We’ve identified four “no-brainer” areas where pharmacists can improve your program’s performance.
1. Transitions of Care
According to a report from the Institute of Medicine on preventing medication errors, the average hospital patient is subjected to an average of one medication error per day.1 While not all medication errors are harmful, about 20% are believed to be.2,3
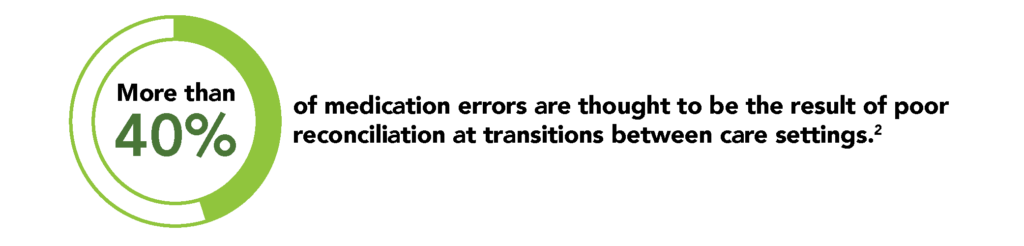
To guard against these errors, ensure that transitions of care always involve a pharmacist to ensure diligent attention is paid to medication reconciliation for every patient.
Medication reconciliation requires a complete and accurate list of all a patient’s current medications. That list must then be compared to medications in the patient’s record or medication orders, which may have changed at transition times (e.g. discharge from hospital).4 This process is designed to avoid omissions, duplications, dosing errors, and potential drug interactions.
A reconciliation should take place at every transition of care when new medications are ordered or existing orders are rewritten, including whenever there is a change in service, practitioner, or level of care. Pharmacists are uniquely qualified to ensure that transitions of care proceed smoothly.
2. Medication adherence
There are many approaches available to improve medication adherence, some simple and some complex. They range from simply calling or texting patients regularly to providing custom packaging designed to support adherence. In any case, if your goal is to improve adherence, pharmacists should be front and center.

Research shows that patients who are prescribed medications for chronic conditions usually don’t take it as prescribed. Within six months of initiating treatment, most are taking less medication than prescribed, or have stopped completely.6 Too often the result is hospital admissions and emergency department (ED) visits. In the end, poor adherence costs U.S. healthcare as much as $289 billion annually.5
It has been shown that putting pharmacists in a position to monitor and advise patients can improve medication adherence by up to 30%. The downstream impact includes reduced 30-day hospital readmissions and reduce ED visits.7
3. Chronic disease management
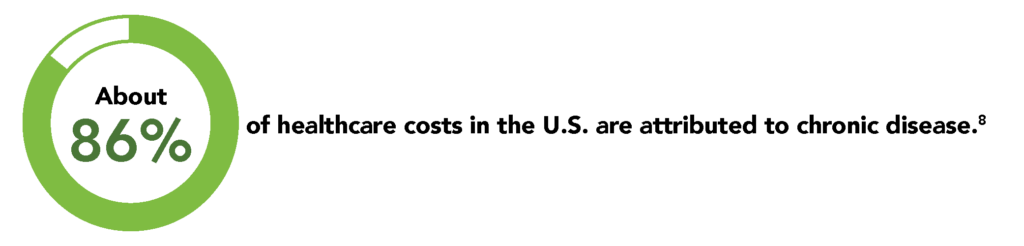
About 86% of healthcare costs in the U.S. are attributed to chronic disease.8 It follows, then, that treating chronic disease also has a significant impact on overworked healthcare providers as well as healthcare institutions that are understaffed.
Consider how often pharmacists are consulted about common ailments like the flu. In many cases they already advise patients who might otherwise seek care from physicians or even emergency departments. In fact, pharmacists are generally well prepared to effectively manage patients who simply need basic monitoring and screening of issues like blood pressure and blood glucose.
Given this fact, pharmacists are beginning to play a greater role in the management of chronic illnesses. Leveraging pharmacists as an extension of the care team delivers considerable benefits to patients, payers, and society at large. VBC organizations should strongly consider leveraging pharmacists’ training and accessibility to improve clinical and financial outcomes.
4. Data Collection and Analysis
Data collection is a foundation of value-based care but the data collected is not actionable until interpreted and leveraged by a qualified professional. Health plans and other health care organizations can work with pharmacists to interpret extensive data regarding patients’ medication use in order to improve the quality and value of care delivered.
Pharmacists are trained to identify safety issues, optimize drug treatment regimens, and prevent medication-related concerns of all types before they become serious problems.
Emerging technologies like pharmacogenomics enhance their ability to assess potential risks and provide personalized guidance to patients. This data can also be leveraged to identify population-wide opportunities for improvement in patient care and to inform broader clinical intervention strategies.
Collaboration and Communication are Key
Ultimately, robust collaboration and communication is the key to success in pharmacist-led care initiatives. When you recognize the contributions that pharmacists can make, and structure care programs with their expertise in mind, your organization, and the patients it serves will see improved clinical and financial outcomes. Pharmacists are ready to extend the reach of care teams, and eager to partner with VBC organizations to deliver the quality care your patients need, together with the value you demand.
Share this: