Medication adherence is widely recognized as a critical factor in achieving positive outcomes for patients and healthcare organizations. When patients adhere to their prescribed medications, they can effectively manage chronic conditions, prevent complications, and achieve better overall health. Furthermore, healthcare organizations benefit from improved patient outcomes, reduced hospitalizations, and decreased financial burdens.
While adherence is a vital element of patient care, a potential downside exists. It’s important to recognize that in some cases, efforts to support patients in taking their medications as prescribed may be inadvertently leading to harmful consequences for patients and healthcare organizations. Make sure your organization isn’t making these mistakes when promoting adherence.
1. Encouraging patients to take medications that are ineffective or potentially harmful.
No clinician intentionally encourages patients to take dangerous medications, nor are they careless in their prescribing habits. Not all medication risks are simple to spot, and it can be challenging for physicians to monitor every detail of every patient’s regimen. A medication alone may not be harmful, but it may interact with another medication, causing side effects that can lead to prescribing cascades. Medications should also be assessed for appropriate duration of therapy, but with patients who may be seeing multiple specialists and providers, clinicians may not detect any issues at a glance.
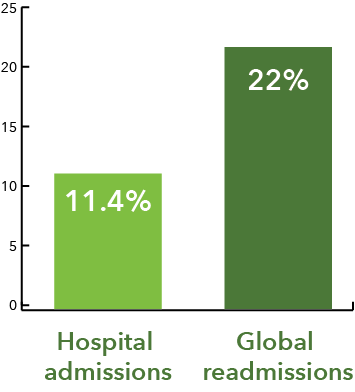
Promoting the wrong medications can also lead to polypharmacy. In a national health survey, the Centers for Disease Control and Prevention reported that nearly one-third of older adults (> 65) take five or more medications.2 Polypharmacy can have severe impacts on hospitalizations and even mortality. In a recent study, researchers reported that up to 11.4% of hospital admissions and 22% of readmissions globally are caused by drug-related events.3 The same study reported that drug-drug interactions are the third leading cause of outpatient visits after cardiovascular diseases and cancer.3
If avoiding this mistake was as simple as taking a quick look at the patient’s medication list, there would be less of an issue. But there is more to it. Having a comprehensive understanding of how a patient’s medications are interacting with one another fosters prescribing habits that can prevent more issues down the road. Using automated tools makes this possible.
2. You don’t have enough information.
In some cases, providers and health plans may have incomplete or limited access to comprehensive patient profiles. Without a holistic understanding of a patient’s medical history, including past medication use, allergies, over the counter medications and other relevant factors, providers may make decisions based on incomplete information. As a result, physicians may prescribe medications that may interact negatively with existing medications or to which the patient has previously experienced non-response or adverse reactions. Failing to consider the complete patient profile increases the likelihood of reinforcing incorrect medication regimens.
3. Maintaining a siloed view of healthcare teams.
Collaboration among a patient’s healthcare team is key to maintaining comprehensive, holistic care. When the healthcare team and patients work together, everyone is aligned, and the patient receives the best possible care. Partnering with pharmacists is a significant step in optimizing medication management. Pharmacists do more for patients than dispense medications; they can provide deeper insights to a patient’s medication regimen and make recommendations that may enhance their medication therapy. (Read more about the role of pharmacists in healthcare.)
Collaboration among healthcare teams benefits quality of care all around, but without patients on board, providers can’t improve adherence. That’s where communication and education come in. Lack of motivation and education are among the top patient-related barriers to adherence.1 Helping patients understand their medications and empowering them to take an active role in their care plan can help you work together to align treatment goals with their health goals.
Leveraging Technology to Support Patient-Centered Approaches
Complex treatment plans add to the challenge of closely monitoring patient regimens and medical history. But thanks to technology, there are efficient ways to enhance medication management. Incorporating clinical decision support systems, precision medicine, and predictive analytics can help health plans and providers stay on top of patient care history and medication regimens by not only holding data but providing clinically based risk analyses and predictions. Using these types of technologies helps organizations streamline operations and empower them to prioritize and optimize patient-centered care.
Non-adherence may be a continuous challenge, but with collaboration, a patient-centered approach, and the right tools to help, healthcare teams and patients together can not only increase adherence rates but improve overall health outcomes. Want to read more on adherence? Click here.
Share this:



